Gastrointestinal causes of chronic pelvic pain
Gastrointestinal problems are a major cause of chronic pelvic pain. They may occur separately, but sometimes they are combined with other pelvic conditions. The most common problems within this group seen in a chronic pelvic pain clinic are IBS and chronic appendicitis. On the other hand, patients with ulcerative colitis or Crohn’s disease usually would have been diagnosed beforehand and are not common customers of a chronic pelvic pain clinic problems are a major cause of chronic pelvic pain.
They could occur separately but sometimes they are combined with other pelvic
conditions. Chronic pelvic pain could be attributed to the following
conditions:
- Chronic
constipation is a common cause of lower abdominal pain but not within a chronic
pelvic pain clinic.
- Irritable
bowel syndrome [IBS] is the most common problem within this group.
- Chronic
appendicitis is usually a neglected cause of chronic pelvic pain.
- Inflammatory
bowel disease [ulcerative colitis and Crohn’s disease].
- Diverticular
disease usually presents as an acute rather than chronic pain.
- Chronic
intermittent intestinal obstruction secondary to bowel adhesions in patients
with previous history of surgery. Pain may be attributed to difficulties in
the free movement of gases and other bowel contents.
However,
the most common problems within this group seen in a chronic pelvic pain clinic
are IBS and chronic appendicitis. On the other hand, patients with ulcerative
colitis or Crohn’s disease usually would have been diagnosed beforehand and are
not common customers of a chronic pelvic pain clinic.
Irritable bowel syndrome
This is a functional bowel disorder
which makes 25-50% of patients’ visits to the gastroenterologists. Symptoms
usually start at a young age. Patients usually present with colicky lower
abdominal pains which are worse after meals and improve after bowel
motions. Bloating and abdominal distension are other common problems. Patients
with IBS could present predominantly with diarrhoea, constipation or
alternating symptoms between the two. However, women are more prone to
constipation rather than diarrhoea. Urgency, passing lots of mucus, change in
the frequency of passing stools or the consistency of the stool itself and a
feeling of incomplete emptying after defecation are also common. Patients with
IBS are more likely to have other pelvic pain generating conditions including
endometriosis [Mathias
et al, 1998]. Some of the criteria used to
exclude the condition include:
- Symptoms appearing for the first time after the age of 50 years
- Presence of constitutional symptoms or significant weight loss
- Pain during the night time and night motions
- Blood in the stools
Usually there are no physical findings
on examination but the sigmoid colon could be palpable and tender in lean
patients. Furthermore, there are no established characteristic imaging criteria
or endoscopic pictures. However, a recent report showed that the sigmoid colon
wall measurement during transvaginal scan examination could be helpful in
excluding IBS. Crade
and Pham [2006]
reported that a sigmoid wall thickness of 3.0 mm gave a sensitivity of 70%,
specificity of 95% and positive predictive value of 73% in diagnosing IBS.
However, more importantly, the negative predictive value was 95% which meant
that a measurement less than 3 mm could almost exclude the diagnosis of IBS. This
could be a very important test in excluding the syndrome which would allow more
effort and time to be diverted to diagnose other possible pathologies. Testing
for food allergies, parasites, lactose intolerance, fructose malabsorption and
coeliac disease is occasionally necessary.
Treatment is usually symptomatic with:
- Antispasmodics
for pain relief.
- Anti
diarrhoeal medication.
- High
fibre diet, lactalose, good hydration and regular exercises for
constipation.
- Dietary
changes to reduce the gastrocolic reflex by using small frequent meals,
soluble fibre food and avoiding diary products. A nutritionist would be
helpful in this respect.
- Tricyclic
antidepressants through their anticholinergic effect could be useful in
controlling IBS symptoms
- Other measures include healthy eating, stress
management etc
Chronic appendicitis
Chronic appendicitis has been seen in
many women with chronic pelvic pain with or without other gynaecological
problems. The appendix was found to be involved with endometriosis in 3.4% -
20% of the cases, when the disease involved other parts of the pelvis, as well [Gustafson et al, 2006 and
Agarwala and Liu, 2003]. In
fact abnormal appendicular pathology was found in many cases with chronic right
iliac fossa pain, even when the appendix looked normal. In 1999 Crose et al reported 11% more abnormal
appendicular histopathology, compared to what could be diagnosed visually.
Paradoxically, they found that 34% of patients who showed improvement in their
symptoms after appendectomy had no related pathology. Accordingly, the appendix
should be removed during laparoscopy in patients with right lower abdominal
pain, even if it looked macroscopically normal. This is the more likely
situation to face endoscopic gynaecologists than cases of acute appendicitis, and they should be able to remove it laparoscopically without difficulty.
Despite the facts mentioned before, specific signs of an abnormal appendix
should be looked for during laparoscopy especially in patients with right side
lower abdominal pains. These signs are:
- Discolouration
- Involvement in
adhesions
- Thick wall on palpation
- Involvement with endometriosis
- The first laparoscopy picture above shows a healthy
looking appendix.
- The second image shows a distended appendix with a thick non-compressible wall, during palpation with a probe.
The patient had chronic right iliac fossa pain, dyspareunia, dysmenorrhoea and dyskesia. She had bilateral endometriomas and endometriosis of the rectovaginal septum. It was too distended to be removed throuhg a 10 mm cannula. Histological assessment of the appendix showed chronic inflammatory cells with no evidence of endometriosis.
The laparoscopic technique for
removing the appendix is a simple one. Following skeletonisation, the base of the appendix is
secured with 2 ligatures with a third one applied just distally. The first
ligature should be applied near to the caecum to avoid leaving behind a long residual
stump which could lead to future attacks of appendicitis. These steps have been
simplified by using pre-tied endoloops which could be applied through a 5 mm
cannula. The
appendix is then transected between the second and third ligatures and
removed in a retrieval bag. This technique would minimise the chances of
any intraperitoneal contamination. Furthermore, securing the stump with two
ligatures would guard against any leakage after surgery.
- The first picture above demonstrates the last stage in skeletonisation of the appendix.
- The second image shows a completely skeletonised appendix.
- The third image shows two ligature loops applied to the base of the appendix.
- The fourth image shows the third loop tightened distal to the second loop.
- The fifth image shows the appendix being cut between the second and the third ligatures
- The sixth and last image shows the appendix stump after being
excised.
Bowel adhesions
Laparoscopy can also reveal many
other bowel problems including bowel adhesions causing bowel tenting, diverticular
disease, and actual involvement of the bowel with endometriosis.
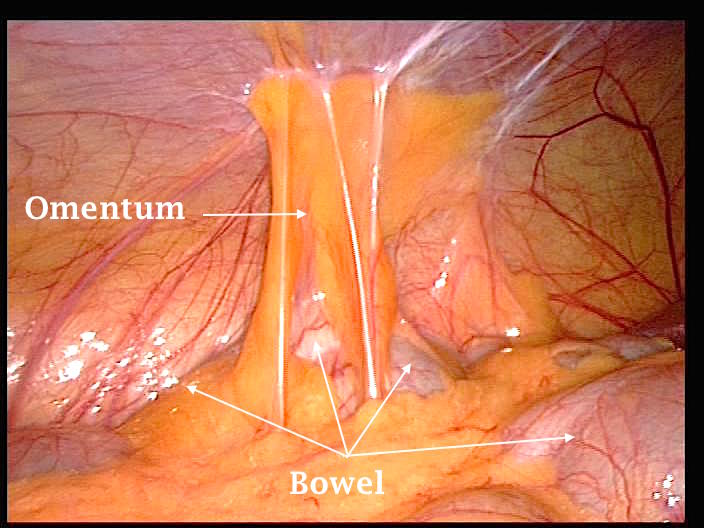
- The first laparoscopic image shown below demonstrates omental and small intestines adhesions to the anterior abdominal wall and the uterus, before being freed. This patient had myomectomy through a sub-umbilical median incision before. She presented with bowel distension, bloating sensation, and frequent episodes of acute lower abdominal pains, not related to menstruation.
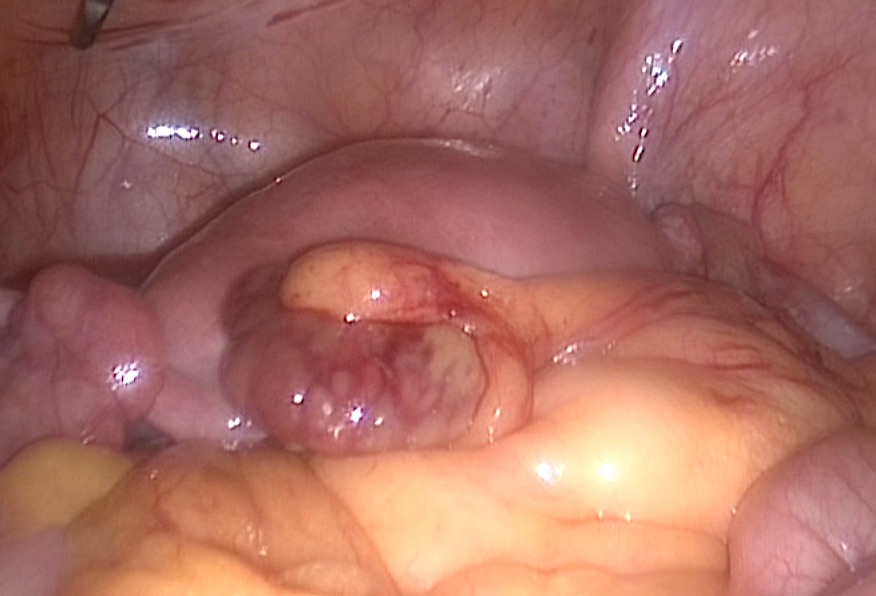
- The second image shows a twisted ileum just before joining the caecum. Th patient had chronic right iliac fossa discomfort and continuous
bloating sensation which settled after surgical correction. The immediate cause for this pathology was not verified even after surgery.
It is noticeable that many women with intense adhesions may not have any pelvic pain or related symptoms. In most of these cases, the adhesions are involving non mobile organs, and are not interfering with blood flow, or gas movement within the intestines. In my experience, I found that adhesions involving small bowel are more likely to give more symptoms, than adhesions involving the large bowel, or the fallopian tubes. Moreover, the initial cause for the formation of adhesions should be taken into consideration. Adhesions following endometriosis or pelvic inflammatory disease are more likely to cause pain than adhesions related to previous surgery.
 |  |
- The first laparoscopic image above shows the sigmoid attached to the anterior and lateral abdominal wall over the left infundibuloplevic ligament. Such adhesions are sometime called congenital, as they are not usually attributable to any obvious cause. I hold a different view as some of these adhesions have no clear line of cleavage from the pelvic sidewall, and show tough scarred tissue during dissection. This may be attributable to infection, or inflammation at that part of the sigmoid colon. This specific patient had no related symptoms and laparoscopy was done during infertility investigations.
- The second image above shows omental adhesions to the anterior abdominal wall, without any significant bowel tenting. This patient also did not have any related bowel symptoms. This is probably due to the fact that bowel movements were not significantly affected by these adhesions
- The first image above shows bowel suspended from a small area lateral to the left inferior epigastric peritoneal fold. This adhesion corresponded to the site of a lateral trocar inserted during previous laparoscopy. Despite the small size of the adhesion area, the patient was much troubled with localised pain in the left iliac fossa, frequent bloating sensation after meals, and occasional sharp pains before and during bowel motions. All symptoms improved dramatically after mobilisation of the bowel. This confirms the already stated point that pain and symptoms related to adhesions are more related to their location and the organ involved, as well as to the initial cause leading to the adhesions formation
- The second image above shows freed bowel with a bleeding scar representing the area of adhesions depicted in the neighbouring image
Inflammatory bowel disease [IBD]
For completion purpose, a summary of these
conditions will be given here. They are a group of inflammatory conditions of
the small intestines and colon, and tend to have more significant symptoms than
IBS. They are usually associated with constitutional symptoms, loss of weight
and blood in the stools.
Crohn’s disease may affect any part of the gastrointestinal
tract from the mouth down to the anus, usually with a skip pattern affecting
some, but not all areas. Though autoimmune and genetic factors may be
involved, the exact cause is not yet known. The whole wall in the inflicted areas
may be inflamed unlike ulcerative colitis, where only the intestinal mucosa is
affected. Symptoms may start anytime between the ages of 15-30 years, with
bloating sensation and abdominal pains. They are usually relieved after bowel
motions. Diarrhoea is also a common symptom, with occasional loss of blood per
rectum. Large volume watery diarrhoea usually follows small intestinal
pathology, where as involvement of the colon usually leads to frequent, but small
bowel motions. It is a usual practice to divide Crohn’s disease into three
different types:
- Penetrating or perforating type, which may lead to abscess and
fistulae formation,
- Stricturing or constricting type causing narrowing of the affected
parts of the bowel, with risk of obstruction,
- Inflammatory type which causes neither of the previous two
complications.
Patients with Crohn’s disease are at risk of
developing systemic medical problems including uveitis, arthritis, erythema
nodosum and primary sclerosing cholangitis. It is interesting to know that smoking
[CosnesJ 2004], and using the oral
contraceptive pill [Lesko et al 1985] may be associated with flare of the disease.
As with all inflammatory bowel diseases,
colonoscopy remains to be the main diagnostic tool. However, involvement of the
upper parts of the small intestines should be investigated with barium studies.
There is no definitive medical or surgical cure for Crohn’s disease, but medical
control can lead to long remissions.
Ulcerative colitis is the other major IBD but is more common than
Cohn’s disease. It has a genetic predisposition as well, but there is no general
agreement regarding an autoimmune cause. As well, diarrhoea and lower abdominal
pain are the main presenting symptoms, with or without systemic problems
involving the eyes, joints, skin, the liver etc. Colonoscopy with biopsies of
the suspected areas is the main diagnostic tool, as the lesions are more
accessible in the lower bowel. Treatment also aims at controlling the
inflammatory episodes, and prolonging the remission periods. However, unlike
Crohn’s disease surgical excision of the colon may cure both the intestinal
and extraintestinal symptoms [Kornbluth and Sachar,
2004].
Diverticular disease
Diverticulosis, or diverticular disease, indicates
outwards submucosal and mucosal protrusions, secondary to colon wall weakness. This can be related to connective tissue problems. There is a
racial difference in the inflicted part of the colon, being more common in the
sigmoid in western societies. However, it is more common on the right side of
the colon in Africans and Asians. It is seen more often in patients 40 years of
age or older, and is associated with obesity, history of constipation and low
fibre high fat diet. It is usually asymptomatic, but may cause left iliac
fossa pain and bloating sensation, with some changes in bowel habits. These are
the usual presentation symptoms in the chronic pelvic pain clinic, rather than
the acute picture seen with diverticulitis, which may develop in 25% of
patients with diverticulosis. In this case,
the patient may present with acute lower left side abdominal pain, with
occasional diarrhoea, and elevated body temperature. Colonoscopy is usually the
best modality for diagnosing diverticulosis. However, it is contraindicated in
cases of diverticulitis, because of the increased probability of bowel
perforation. In this case MRI and CT scanning are very sensitive in localising
the inflicted sites, and the likelihood of any abscess or fistula formation.
Treatment of all bowel related problems is the
remit of the Gastroenterologist and Colorectal Surgeon colleagues in the
chronic pelvic pain management team. However, Gynaecologists should be aware of
the differential diagnosis, to avoid unnecessary gynaecological interventions, and to be able to make the necessary referrals.
Unusual intestinal findings during laparoscopy done for chronic pelvic pain
 | 
|
- The first laparoscopic image above shows a severely congested sigmoid colon, with very prominent blood vessels. There was no sign of diverticulitis, or any local inflammation. The patient had chronic pelvic pain for almost one year. She had thorough investigations including colonoscopy and CT scanning, with negative findings. The sigmoid was freely mobile. Unfortunately, she was lost for follow up.
- The second image shows a gangrenous epiploic appendage with an intact fat pedicle, also rising form the lower part of the sigmoid colon. This patient had another similar one, but less discoloured during the same procedure. She gave history of repeated chronic lower abdominal pains, and perineal discomfort for the previous 6 months. This was accompanied by few episodes of central sharp lower abdominal pains. The image above excludes, the possibility of torsion of the carrying pedicle, which looks normal. Histopathological assessment showed fat necrosis without any evidence of inflammatory cells. A diagnosis of vasculitis was most likely. The patient had complete pain relief following the procedure, and is currently under investigation to ascertain the cause of spontaneous intestinal fat necrosis.



