What is Pain?
Pain was described as: 'An unpleasant sensory and emotional experience, associated with actual or potential tissue damage' by the International Association for the Study of pain. It is described as pelvic when its localised in the true pelvis, abdomen below the umbilicus, or lower back. It has the following characteristics:
- It is a subjective feeling, hence patients complaints should be accepted as real.
- There are no objective means to confirm its existence, or assess its intensity.
- It can be acute or chronic, as verified by many characteristics, including duration.
Acute pain
Acute pain should be considered as an immediate physiological protective feeling, following localised tissue injury. Usually it has no lasting major effects, but may be associated with temporary mild distress and anxiety. It should be considered as a defensive mechanism, as well. Certain changes in motor and psychological behaviour will be initiated by the brain, to limit the extent of injury. It is usually localised to the injured part of the body, and its physical characteristics are easily describable by the patient. It usually has a short duration, and resolves by the time of tissue healing.
Chronic pain
Chronic pain, on the other hand, has been traditionally diagnosed when pain persisted for 3 months, or cyclically for 6 months duration. However, recently 6 months became the standard period to make the diagnosis, but few articles excluded cyclical pain from the definition. It is noticeable that both definitions put all emphasis on the duration of the pain, which is not the main issue to consider when differentiating between the two types. It is the author's opinion that cyclical pain, in the form of dysmenorrhoea is one of the very important presentations of endometriosis, together with cyclical ovulation pain. Excluding such symptoms will put many patients at risk of a wrong, or at least delayed, diagnosis, and management. Furthermore, in my view using the terms primary and secondary dysmenorrhoea, in almost a diagnostic manner, also added to the problem. It is usually suggested that primary dysmenorrhoea is a simple problem, and most women will be cured after childbirth. On the other hand, it is more important to know that 70% of women with endometriosis date their symptoms back to their pubertal years, if not exactly to menarche. So pubertal pain should be considered as an important possibility for the presence of endometriosis, especially if combined with other related symptoms, like diarrhoea and bloating sensation.
Unlike acute pain, the chronic type usually lasts longer than normal healing time, and has no physiologically protective role. Furthermore, patients usually find it difficult to describe the exact characteristics, and exact location of the pain. More important, it affects the quality of life, and often has a psychological cause, or effect. In most cases, multiple rather than one factor may be involved in causing the pain. Because of all these special characteristics, chronic pelvic pain is now considered to be a pathological entity by itself.
Pain origin
Pain can be of cutaneous, somatic or visceral origin caused by stimulation of pain receptors [nociceptors], which decline in number in these respective tissues. Differences in receptors number is important in determining the type and intensity of pain perceived in these areas. Cutaneous pain has a sharp quality, as it is conveyed by the fast A-delta fibres. On the other hand, pain from deeper areas is conveyed by slower C-fibres leading to poor localisation. However, an overlap in the quality of pain is not unusual.
Pain can be neuropathic in origin produced by different pathological means, not involved with nociceptive or inflammatory types of pain. It may follow sensory nerve fibres injury, or damage to the central nervous system itself. Patients may describe it as a burning or electric sensation, and is usually worst at night time. It may also follow prolonged peripheral nerves stimulation. This usually lead to sensitisation of the respective area, resulting in pain out of proportion to what is expected after true tissue damage. This is called primary hyperalgesia. On the other hand, sensitisation of the dorsal horn receptors may lead to secondary hyperalgesia, causing pain in normal areas neighbouring the injured nerve. Patients can also feel pain in response to non-painful stimuli. This condition is known as allodynia. Finally, neuropathic pain may be referred from one viscus to the other, or to a cutaneous or muscular area not involved in the initial pathological process. This is known as viscero-visceral and viscerosomatic conversion respectively.
The objectives of writing this manuscript are:
- To increase the awareness of primary care providers and gynaecologists to the magnitude of the problem in the society, and to encourage patients to come forward for assessment especially teenage girls, and women with adult onset pain.
- To introduce questions about pelvic pain during all consultations, bearing in mind that women are usually less likely to volunteer this information, even by inner city areas liberal women.
- To discuss the characteristics of the different types of pain, and how they can interchange in the same patient, over long periods of time.
- To stress the importance of multidisciplinary teams, bearing in mind that many factors, rather than one may be involved in the causation of pain.
- To be aware of the different psychological issues and phobias involved with each individual case. Younger women are more concerned about their fertility potential, where as fear of cancer is the main issue in older patients. These issues form a substantial psychological burden in the minds of many patients with chronic pelvic pain.
- To emphasise the need for a disciplined approach with formalised structured management protocols and follow up procedures. This will reduce unnecessary investigations and ineffective empirical treatment. This can only improve patientsí confidence and compliance.
- To be more proactive with patients, their families and primary care providers. This will close all gaps in patients' management, and reduce frustration and relapse. It is important to remember that such patients are liable to feel neglected and lonely.
- Patients are more likely to open up and talk about their problems, when not escorted by a parent or another person. It may take more than one visit to the clinic before the patient can talk liberally about her problem.
- It is more likely to get more information about sexual abuse and other personal problems from the questionnaires filled by patients, than during official interviews.
Chronic pelvic pain
No age group is immune against chronic
pelvic pain. With an annual prevalence rate of 38/1000, it is as common as
asthma, migraine and lower backache. However, the monthly prevalence rates
increased with age from 18.1/1000 in 15-20 years olds to 27.6/1000 in women
older than 60 years [Zondervan
et al, 1999 a]. The
exact prevalence is different in different societies but a figure of 20% is a
reasonable average across different age groups. It makes 10% of all
gynaecological visits [Reiter
RC, 1990], 40% of all laparoscopies [Howard FM, 1993] and 10-20% of hysterectomies are
usually done for pelvic pain. As well gastroenterologists, urologists,
colorectal surgeons and back pain specialists spend considerable time in their
respective practices dealing with patients presenting with recurrent episodes
of pain.
Patients with psychological problems are more prone to develop chronic
pelvic pain. It is worth noting that history of sexual or physical abuse has been reported in 40-50%
of the cases [Walker
et al, 1988; Rapkin et al, 1990; Reiter and Gambone, 1990; Jamieson and Steege,
1997 and Collett et al, 1998]. However, the author of this book dealt with thousands of patients from different communities, who presented with chronic pelvic pain, yet can not confirm that sexual abuse was a regular point in the previous or presentation history. May be, we practice in a different culture, and different time to the reports published in the eighties and nineties. Patients were usually asked for such history by a female and a male member of staff, at different times. As well, each patient had to fill a pain questionnaire which addressed this question, by her own without any help from her family. We use a female member of staff for the intitial history taking, as we found many patients open up more readily to female staff members, in the absence of any family member. Such question was usually tactfully repeated in a later visit, after gaining the patient's confidence. This again was usually done without a parter or another member of staff being present.
Other reported factors predisposing to chronic pelvic pain included personality, marital and childhood disorders as well as
depression and anxiety state. Unfortunately, dealing with these patients in
real life is far from ideal. About 60% of them were not referred for specialist
care, and 28% never received a diagnosis, 3-4 years after their first
consultation. This information is based on a MediPlus UK Primary Care Database study involving 136
general practices [Zondervan
et al, 1999 b]. In 2004 Stone W discussed the attitude of general
practitioners, gynaecologists and patients as related to this problem. General
practitioners found it difficult to deal with patients who had no definite
diagnosis, and needed long and repeated consultations. As well, they were aware
of a general lack of interest by gynaecologists to deal with this problem. Accordingly, they had difficulty in finding the right specialist for the job. On the other hand,
gynaecologists usually needed to see some form of pathology to react to the patientsí
symptoms. Furthermore, they were reluctant to raise psychological issues with
their patients, most likely due to lack of training in this area. At the same time, restrictions in specialists busy clinics usually
reduced their ability to give the necessary time needed by these patients.
As for patients, they expected to have long frequent consultations with
detailed explanations, continuity of care, and most important a diagnosis to
explain their sufferings. This was not a unique problem in Britain as the
American Endometriosis Society released almost similar findings in
2002. This showed a common lack of
structured care to deal with this problem in two leading Western Countries. Accordingly, one expects a similar attitude, if not even worse, in most parts of the world.
I was surprised by two emphatic statements from doctors in two Middle Eastern countries to the effect that chronic pelvic pain was not a common problem they encountered. The other statement was that endometriosis was very rare indeed, in their communities. In reality, I found the opposite to be true in relation to the two statements. Most of my work during my short stay, then, was dealing with such inflicted patients. This may relate to the same apathy shown by doctors in the Western Countries, but limited endoscopic surgery training may be a strong factor, as well. Cultural factors are also important, and should be tackled. Women tended to be shy to speak about periods pains, and pain during intercourse or defaecation. Accordingly, part of the protocol we established included specific questionnaires to ask about such problems, even in women presenting for contraceptive advice, or unrelated gynaecological issues. It is not uncommon for patients to present with a request for 'general check-up', with the real cause for the visit to be revealed some time during the interview as pelvic pain, dyspareunia or dyskesia. We have to understand the cultural background of our patients. In one community women may complain readily of abdominal and pelvic pain, where as the real cause for the visit was inability to conceive.
To combat this apathy,
dedicated multidisciplinary teams are needed for the proper diagnosis,
management and follow up of patients with this complex problem. To deal with
these patients, the teams involved should adopt the following general
principles:
- Listen to the patient, show interest in her problems and provide
good explanations, when possible. It has been shown that a patientís
impression of her first consultation and how the physician was sympathetic
to her cause had great bearing in her recovery.
- Note should be taken of the entire patientís previous medical and
surgical, history. The indications for pervious surgery, exact findings
and pathology diagnosed as well as the procedure performed should be
ascertained.
- Always think of different causes, rather than one cause for chronic
pelvic pain. Identifying and treating one pathology is unlikely to be
successful [Butrick
CW, 2007]. Always try
to identify all pain generators and deal with them in a total pain
management plan. This entails treating the underlying conditions as well
as controlling the pain itself with the appropriate means.
- Try to find and assess the magnitude of any predisposing or
associated psychological factors which may have an important bearing on
the management of these patients.
- Set realistic management goals and plan, and avoid unnecessary
surgical interventions. Pain control may be the best option available
rather than absolute cure in many cases. Patients should be made aware of
this possibility.
- Carry all objective investigations as soon as possible to make a
reliable diagnosis. One should bear in mind that management of illness may be
more important than identifying a single pathology, which might not be the
real cause of the problem.
- Intervene early when indicated to prevent the development of the
chronic pelvic pain syndrome.
- Stick to the agreed protocols to avoid conflict of opinion within
the multidisciplinary team which can send the wrong message to an
already confused and stressed patient.
- The team should have regular meetings to discuss cases and audit
outcome.
Having said that, it is also very important in the first place to convince young patients with pelvic pain to seek specialised medical advice. It is not uncommon, for mothers to describe similar sufferings they had during their younger years, and how they grew out them with time, or after marriage. It is stated some where else in this book that many women with endometriosis dated their symptoms back to their teenage years. In my view, it is an obligation of the medical community to educate the public regarding pelvic pain and an especially endometriosis. This can be done in schools, family clubs, and through the media.
Impact of chronic pelvic pain on the patient and
her family
With
all types of chronic pain, patients are at risk of poor physical and mental
health. This may lead to:
- Loss of quality of life and reduced
ability to relate to other people.
- The patient may feel isolated and her
symptoms not appreciated by her own family and friends. Many of these
patients may have an abnormal scoring in mental health questionnaires.
- Inability to work or perform any
physical exercise
- Tendency to take frequent sick leave or
absent herself from work
- Reduced productivity even if she
attended for work
- Increased risk of unemployment
- Loss of income with changes in
standards of living
- Tendency for repeated attendance to
causality departments
- Risk of unnecessary surgical
interventions
Management plan logistics
The ultimate objectives in dealing with
patients with chronic pelvic pain are:
- Provide adequate pain relief and reduce the frequency of pain
episodes.
- Identify the possible sources of pain and deal with them either
medically or surgically.
- Improve the quality of life to allow the patient to lead a normal
or as near normal life as possible and to function normally in her family
and society.
- Deal with any predisposing psychological factors or other current
concerns which are worrying the patient. Young women are usually concerned
about future fertility problems and older ones are worried about the risks
of having a hysterectomy and cancer.
- Prevent the development of the chronic pelvic pain syndrome.
To fulfil these objectives a
multidisciplinary team with a lead clinician should be involved in dealing with
patients with chronic pelvic pain. The group should include:
- A nurse co-ordinator as the liaison person in the group
- A gynaecologist as the lead clinician
- Gastroenterologist
- Colorectal surgeon with minimal access surgery interest
- Urologist with minimal access surgery interest
- Psychologist with special interest in pelvic pain
- Physiotherapist with special experience in chronic pelvic pain
- Pain specialist usually an anaesthetist
- Nutritionist
It is important that all members should
have special interest and training in dealing with these patients. Furthermore,
an objective structured plan should be used for diagnosis and follow up. Pain
calendars and pain questionnaires with diagrams for pain mapping are the
starting points but should not replace the clinical consultation which should
last for one hour on average to be inclusive. During such interviews important
and doubtful points identified in the patientís response to the questionnaire
should be verified. As well the clinician would have a good chance to establish
a rapport with the patient and judge the magnitude of her problems. The
questionnaire should be broad based to explore all sorts of psychological
problems including fertility concerns in young women and fear of cancer in
older patients. History of physical and sexual abuse should also be documented.
Pictorial mapping could show pain distribution along specific myotomes or
dermatomes identifying musculoskeletal and extra pelvic pain sites. Always try
to be objective in quantifying the patientsí symptoms by using visual pain
scale. This would be most helpful in assessing the magnitude of change after
any form of treatment. It is not unusual to need two or three clinical sessions
before a patient would reveal her real concerns and the important points in her
past history which might have had some bearing on her condition. It is
important to look at the questionnaire and clinical consultations as
complementary methods to evaluate the patientís condition and plan her future
management rather than considering them as alternatives.
A structured physical examination in
the erect, sitting, supine and lithotomy positions should be done as the pain
could well be of non-gynaecological origin. Special attention should be given
to standing, walking and sitting postures. A typical posture of
patients with chronic pelvic pain is manifested with excessive lordosis
and forward pelvic tilt with difficulty in correcting the lumber curve on
forward bend. They
usually sit at the edge of the chair or lean on one thigh or the other in cases
of vulvodynia and pelvic floor tenderness. A recent study in Norway examined
posture and movement patterns in women with chronic pelvic pain [Haugstad et al, 2006]. Both parameters were significantly
worse compared to a healthy control group. Hernias should be looked for while
the patient is standing up. Examination for excessive lordosis, scoliosis and
asymmetry of the pelvis should be done. Abdominal examination for surgical
scars, swellings, tenderness and guarding is necessary. Special attention
should be paid for localised tender trigger points along all the anterior
abdominal wall muscles. With abdominal tenderness, Carnettís sign should be
elicited. It entails that pain which decreases after tensing up the abdominal
muscles is usually of intra abdominal origin. On the other hand, pain which
increases or at least stays the same during this test is of muscular origin.
However, inflammation of the parietal peritoneum beneath the tender area could
give a false result. Pelvic examination should be started with good inspection
of the vulva and vestibule and Q-tip test for vulvovestibulitis. This should be
followed by single digit examination to check for a tender episiotomy scar if
applicable, tender robe-like urethra or bladder bed and to palpate the
pubococcygeus, ischeococcygeus, coccygeus overlying the sacrospinous ligament
and obturator internus muscle more anteriorly for tenderness. The cervix should
be moved from side to side to elicit any excitation tenderness. This could be
secondary to pelvic peritoneum irritation with endometriosis, blood or
infection. Bimanual pelvic and rectal examinations should be the last to
perform and should preferably be done during menstruation to look for tender
induration of the rectovaginal septum, pouch of Douglas or uterosacral
ligaments which would be missed in 40-50% of the cases if done at other times.
It could as well reveal uterine and adnexal abnormalities.
Investigations should include a
temperature chart in adolescent girls to look for sustained temperature during
menstruation which could relate to endometriosis. A blood test for FBC, ESR,
and C - Reactive protein as well as a urine sample or endocervical swab for
chlamydia should be done to explore the possibility of pelvic inflammatory
disease. A blood test for chlamydia antibodies, IgM, is not as sensitive as the
previous two tests in diagnosing acute infections but a high IgG level is very
useful in exploring the possibility of previous infection. Other investigations
include transvaginal scan examination, MRI especially for adenomyosis and
endometriosis of the rectum and sigmoid colon. More information would be given
latter on in this chapter.
The role of laparoscopy in chronic pelvic pain
Despite the great advances in the different types of imaging, laparoscopy remains to be the most sensitive method in the diagnosis of chronic pelvic pain causes. Previous studies showed different pathological findings after diagnostic laparoscopy compared to physical examination and imaging studies. Kang et al in 2006 reported that 42.7% of the patients who had diagnostic laparoscopy, had their management plan set by clinical and imaging findings changed. This is rather a high percentage, and may entail liberal use of diagnostic laparoscopy, as a primary diagnostic tool. Alternatively, it may show less clinical acuity in making the initial diagnosis, and puts forward the question at what level of experience that diagnosis was made? This figure must definitely be lower in units using set protocols and standard procedures, within a multidisciplinary practice.
It is almost agreeable across the board that laparoscopy is indicated early for the diagnosis and management of patients with positive physical signs on clinical examination. Otherwise, specific selection criteria should be set to avoid unnecessary surgical interventions. It can be recommended in the following situations:When the symptoms have already affected the quality of life, being social, marital or professional.
- When the initial medical treatment has failed to offer complete pain relief or progressively higher doses of analgesics are needed to maintain comfort.
- For treatment purposes of an already diagnosed pathology using imaging techniques
- There are new symptoms after initial surgical treatment.
- Infertile patients with chronic pelvic pain are a special group who should be examined early. Milingos et al [2006]reported their laparoscopic findings in 369 and 1215 infertile women with and with no chronic pelvic pain respectively. Pelvic pathology was diagnosed in 76.7% and 42.6% in the two respective groups. Omental adhesions, hydrosalpinges with pelvic adhesions, severe endometriosis, pelvic congestion and endometriomas were significantly more frequent in the infertile group with chronic pelvic pain.
It is important to mention that finding pelvic pathology during laparoscopy does not prove causation as endometriosis has been found in 45% of asymptomatic patients [Rawson JMR, 1991]. Furthermore, it has been shown that patients with chronic pelvic pain and those with asymptomatic infertility had similar findings during laparoscopic assessment [Palter et al, 1991; Rapkin AJ, 1986; Stout et al, 1991 and Walker et al, 1998]. On the other hand a negative finding during laparoscopy does not prove normality as 35% of patient with chronic pelvic pain may have no visible pathology [Cheong and William Stones, 2006]. This can be due to:
- Non classical endometriosis, or if laparoscopy was performed after medical treatment with GnRH- analogues, continuous oral contraceptives or progestogens
- Deep endometriosis in the rectovaginal septum is more palpable than visible
- Functional bowel problems
- Pelvic congestion concealed with the head-down position, and high intra abdominal pressure sustained by pneumoperitoneum during laparoscopy
- Musculoskeletal disorders
- Missed inguinal or other hernias
- Missed chronic appendicitis or chronic inflammatory bowel disease
A prospective study published by Nascu et al in 2006 documented the histological findings in excised uterosacral ligaments from 27 patients with chronic pelvic pain and normal findings on visual inspection during laparoscopy. Endometriosis, endosalpingosis, and inflammatory changes were diagnosed in 17 patients (63%). Furthermore, there was significant improvement in patients symptoms mainly dysmenorrhoea, dyspareunia and noncyclic pain.
The incidence of positive identification of endometriosis after diagnostic laparoscopy is very different in different series. In a review of 1524 laparoscopies done for chronic pelvic pain, endometriosis was seen in 33% of the cases, pelvic adhesions in 24%, chronic pelvic inflammatory disease in 5%, ovarian cysts in 3%, pelvic varicosity and fibroids in <1% each. Variable pathologies were seen in 4% and no pathology was reported in 35% of the cases [Howard FM, 1996]. On the other hand Mara et al in 2002 documented their results after 480 diagnostic laparoscopies were done for pelvic pain. Endometriosis, normal findings, pelvic adhesions and PID were seen in 20.4%, 17.7%, 22.3% and 17.7% of the cases respectively. Special note should be taken of the differences in the incidence of PID between the two series (5% vs. 17.7%). In contrast, Kang et al in 2007 reported a 60.2% positive identification rate of endometriosis after 3068 diagnostic laparoscopies performed for chronic pelvic pain. A normal pelvis with no obvious finding to explain the pelvic pain was seen in 21.1% of the cases. Such differences between the various studies may be a reflection of the selection criteria used by the different authors before patients were subjected to diagnostic laparoscopy. They may as well reflect differences in the criteria used to diagnose endometriosis, or real differences in the incidence of endometriosis, PID and other causes of chronic pelvic pain, among different populations. Taking note of the incidence of endometriosis in the 3 studies quoted above shows wide gaps between 33%, 20.4% and 60.2% respectively. The message to learn at this point is that, different populations may have different disease patterns. Accordingly, proper clinical diagnostic protocols should be adopted, with set criteria for diagnostic laparoscopy and continuous auditing of results, to avoid unnecessary interventions with high negative findings.
To cater for the negative findings during laparoscopy, conscious pain mapping under local anaesthesia and sedation has been advocated first by Peter et al [1996], and further explored by others including Howard FM, [2000] and Howard et al [2000]. During the procedure different parts of the pelvis were palpated with a thin probe and assessed for reproduction of the patientís symptoms in a proactive way. Reports showed that thin filmy adhesions involving the bowel can give more pain than thick adhesions in other areas. However, further studies are needed for full evaluation of this technique.
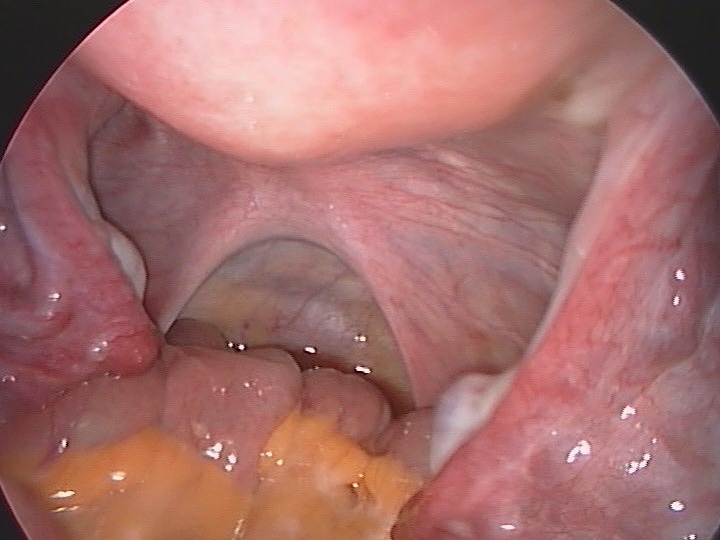 |
The laparoscopic image shown above reveals a normal and healthy looking pelvis, with pink peritoneum. There are no signs of adhesions, endometrisosis or pelvic inflammatory disases. The pouch of Douglas also looks normal, with distinct normal looking uterosacral ligaments, on each side. This patient had laparoscopic examination during infertility investigations. Any deviation from such an appearance may indicate some sort of abnromality, but not necessarily as a casuse of pelvic pain.