| Ovarian and adnexal masses
Ovarian cysts and adnexal masses are common incidental findings during pelvic scan examinations. However, they are more likely to cause acute pelvic pain because of accidental rupture or
complete torsion. On the other hand, repeated partial or incomplete torsion
episodes, leaking into the pelvis or bleeding within the cyst itself can cause intermittent episodes of pelvic pain. Furthermore, the nature of the cyst and
adnexal mass may have a bearing on their mode of presentation. Endometriomas may cause pelvic pain, mostly peri-menstrual, especially if attached to the side pelvic wall, or associated with endometriosis in other areas in the pelvis. On the other hand, inflammatory adnexal masses may lead to chronic ill health and
intermittent or chronic pelvic pain. Though the
role of surgery is clear in cases of acute pelvic pain caused by adnexal
masses, its role in the treatment of patients with adnexal masses and chronic
pelvic pain is not as clear. Sadly, ovarian malignancy is usually a silent
pathology, till late in the history of the disease. Accordingly, this possibility should always be kept in mind when dealing with patients with an adnexal mass. The following
points should be ascertained in such cases:
- The origin, size, shape, outline and exact location of the mass and
whether it is unilateral or bilateral
- Wall thickness, echogenicity and the presence of internal wall
irregularities
- The internal features characteristics and echogenicity e.g.
presence of septae or solid and fluid parts
- Posterior shadowing or acoustic enhancement
- The ability to identify the ovary separately from an extra ovarian
mass
- The presence and characteristic of any pelvic or peritoneal fluid
- Doppler characteristics of the mass and the presence of
neovascularisation
- With a suspicious mass the liver should be scanned for any abnormal
shadows.
The ultrasound image shown below
demonstrates a shadowing right ovarian mass. The second picture shows a solid mass attached to the lower pole of the same ovary, as seen during laparoscopy. The third picture shows the same ovary after laparoscopic excision of the solid mass, which proved to be a spindle cell tumour. This patient presented with intermittent episodes of sharp right iliac fossa pain for more than one year.
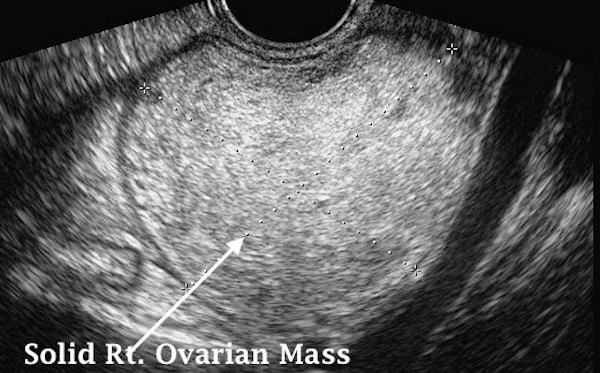
The neighbouring ultrasound image shows a large solid ovarian mass, which also proved to be a spindle cell tumour. Despite the large size, the patient had minimal dull aching pains for more than 2 years. Probably, because the large tumour size and its impaction in the pelvis did not allow the ovary to move or twist on its pedicle.
Tubo-ovarian complex and Abscess It is essential to differentiate between an an inflammatory adnexal complex and an abscess. This is important for setting the management plan in each case. With an inflammatory adnexal mass, the treatment is usually conservative with antibiotics, while an abscess always needs drainage. Ultrasound scan examination may have a good role to play in making the diagnosis in such cases. With a tubo-ovarian complex, the ovary is easily identifiable from the inflamed tube, where as no line of demarcation is identifiable between these two structures in case of an abscess.
Ovarian remnant syndrome
Ovarian
remnants syndrome refers to a condition when small pieces of ovarian tissue
have been left behind after difficult oophorectomy. This is most likely to
occur in cases of severe endometriosis or pelvic adhesions following previous
surgery or PID. It has also been reported after laparoscopic oophorectomy
possibly because of technical difficulties or improper tissue extraction [Nezhat et al, 2000]. The true incidence of the
condition is not known, but it can lead to cyclic pelvic pain or even cause a
pelvic mass. Such patients may not show any hypo-oestrogenic symptoms or
signs, and may even have normal serum oestradiol levels. Transvaginal scan examination
may reveal the diagnosis, but occasionally MRI may be needed for that
purpose. Depending on the size and location of the ovarian tissue left behind
and the extent of pelvic adhesions, laparoscopic localisation and easy access
to the remnant ovarian tissue can be difficult or even impossible. However,
several reports documented safe excision of such ovarian tissue
laparoscopically [Abu-Rafeh et al, 2003; Mahdavi et
al, 2004 and Kho et al, 2007]. On the other hand, Magtibay et al [2005], have also documented a
surgical intraoperative complication rate of 9.6% with
subsequent need for re-exploration in 9.0% of their patients. Despite all the
risks involved, surgical removal of the ovarian remnants is necessary to
alleviate the patientís symptoms, as endometriosis was diagnosed in 29% of such
cases by the last authors. Furthermore, benign serous neoplasia has also been
reported in 3 cases after laparoscopic excision of ovarian remnants by Madhavi et al [2007]. More seriously, some
malignant changes were reported by Kho et al [2007]
in two of their patients. With all this in mind, patients should be counselled
properly and asked to sign the consent form with all the risks involved
thoroughly explained. They should also consent for laparotomy to cater for any
complication or difficult access to the pelvic sidewall. In such difficult
cases a retroperitoneal approach to remove the entire ovarian remnant should be
adopted.
It
may be useful in certain cases to use an oral contraceptive pill or a GnRH-a
to suppress ovulation and give some pain relief. This can be used while the
patient is waiting for surgery, or by patients with a high surgical
risk.
Trapped or residual ovary syndrome
This is
the condition when a conserved ovary causes pelvic pain, deep dyspareunia or
even forms a pelvic mass. An incidence of 2.85% was reported in a large
retrospective case controlled study of 2561 patients who had a hysterectomy
with 46.6% subsequent exploration rate within 5 years and 75.4% by the end of
10 years. [Dekel et al, 1996]. As for all
other ovaries, trapped ones can develop any form of ovarian pathology
irrespective of the presence of the uterus or not. However, they are more prone
to get stuck to the vaginal vault or pelvic sidewall, or both because of pelvic
adhesions. Deep dyspareunia may be the main problem and similar pelvic
tenderness can be elicited during pelvic or transvaginal scan examinations.
Scanning may reveal normal looking ovaries or any other pathology including
endometriomas or other ovarian cysts. The same authors mentioned above reported
functional cysts, benign neoplasm and ovarian carcinoma in 50.7%, 42.6% and
12.3% respectively in the removed ovarian specimens following subsequent
exploration of symptomatic patients. Despite these high percentages in
symptomatic women, the reported incidence of malignant changes among patients
with preserved ovaries as a whole was only 0.25%, which was not different from
the general population [Hwu et al, 1989].
Ovarian
suppression with the combined oral contraceptive pill or a GnRH-a can relieve
the pain but surgical mobilisation of the ovaries or oophorectomy may be
needed for permanent cure in women with severe symptoms. Such suppression may identify those patients who can benefit from surgical intervention and help
in avoiding difficult and unnecessary surgical interventions in women who may not have significant pain relief [Carey and Slack,
1996]. Other than relieving patientsí symptoms, removing the ovaries may have other advantages related to prevention of ovarian cancer as well as
reducing the risk of breast cancer. On the other hand, certain disadvantages
should be taken into consideration before removing both ovaries. A long list includes increased risks of osteoporosis and hip fractures, cardiovascular
disease, impaired short memory and dementia, lower sexual function and
psychological wellbeing [Shoupe et at, 2007].
It is clear that more risk assessment should be practiced, as 78% of women
between the ages of 45-64 years had prophylactic oophorectomy during
hysterectomies done for benign disease to prevent the development of ovarian
carcinoma, as reported by Parker et al, in 2007.
They also reported some statistics using a hypothetical cohort of 1000 women
who had bilateral oophorectomy between the ages of 50-54 years. The benefit
expected was 47 fewer women dying of ovarian cancer but 838 more women would have died of coronary heart disease and 158 more from hip fracture by the
age of 80 years. In percentage terms the increased risk of dying from ovarian
cancer if the ovaries were conserved was 0.47% against 8% more survival rate
due to fewer women dying of cardiovascular disease by the age of 80 years. The
survival rate was 4% more if surgery occurred between the ages of 55-59 year
with no benefit of conserving the ovaries after the age of 65 years [Shoupe et at, 2007]. These beneficial changes of
conserving the ovaries during hysterectomies reflect the fact that
postmenopausal ovaries still produce variable amounts of androgens which are converted peripherally to oestrone, which is a weak oestrogen. |



